I’ve only had hypothermia once in my life. I was nine years old and swimming in a KOA camp pool alone. The sun set and, as it does in the mountains, the temperatures dropped suddenly. When I got out of the pool, I was so cold that I couldn’t move. I began to shiver uncontrollably and felt so weak that I couldn’t move. My skin started turning pale and my lips were blue.
Luckily, my case of hypothermia was mild. After getting into dry clothes, bundling up, and eating lots of chocolate, I was fine. But the experience taught me how easy it is to become hypothermic – especially if you get wet. Because of evaporative cooling, you can get hypothermia even when it isn’t that cold out.
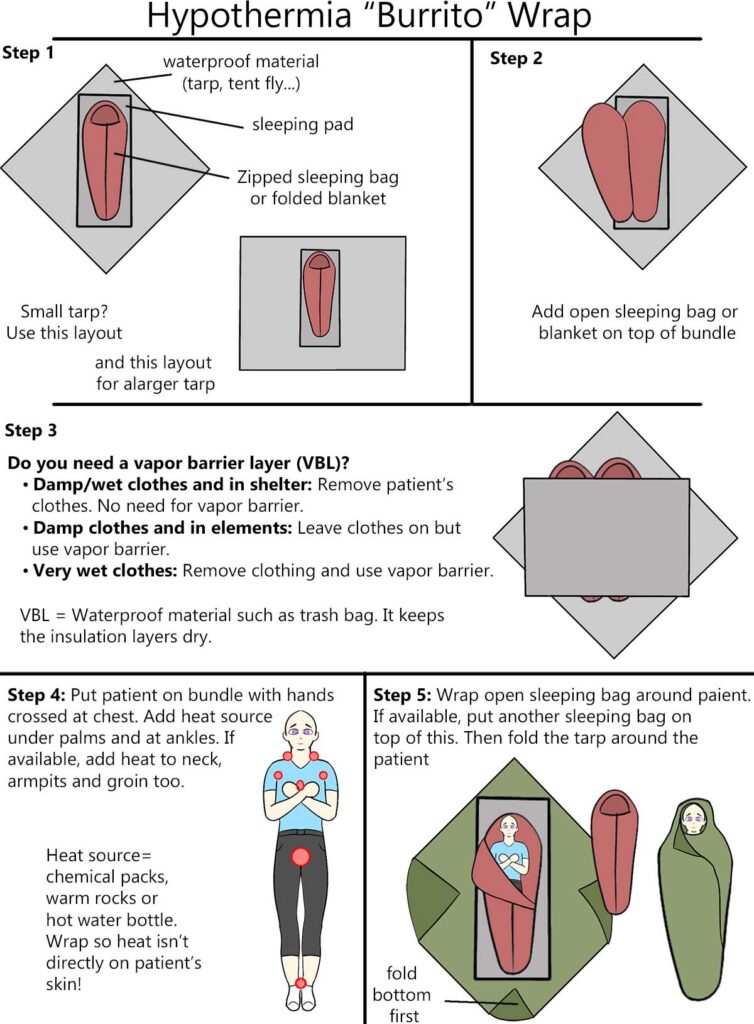
Surprisingly, most hypothermia deaths occur at temperatures of 30 to 50F, probably because people don’t realize there is a danger at these “warmer” temperatures. Thus, if you are going into nature, it is particularly important that you know how to treat hypothermia in the field. I’ll go over the steps in detail. You can see the infographic for the hypothermia “burrito wrap” below.
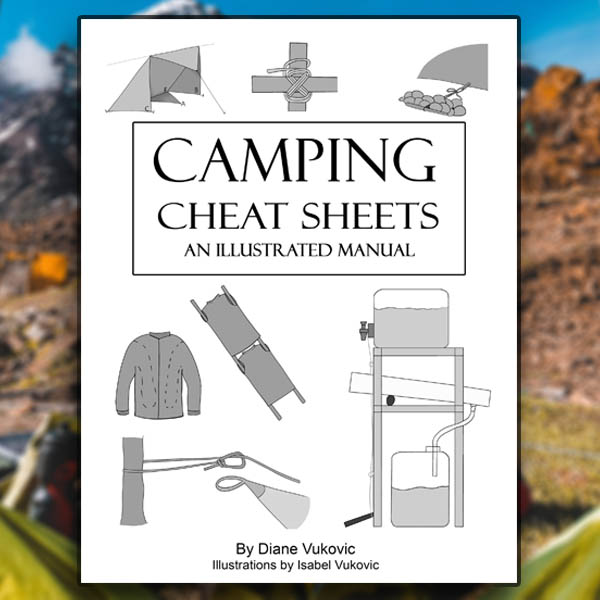
Want these instructions (and more) in PRINTABLE format? Get my Camping Cheat Sheets.
There are 42 illustrated pages that cover wilderness first aid, tarp shelters, fire lays, and more.
How to Treat Hypothermia in the Field
Mild Hypothermia
Symptoms:
- Core body temperature 90-95°F
- Patient is still alert but drowsy
- Violent shivering and chattering of teeth
- May have trouble speaking
- Pale or bluish skin and lips
- Rapid heartbeat and breathing
Treatment:
To treat mild hypothermia, you need to get the patient dry and warm as soon as possible. Remove wet clothing, put the patient in dry clothing, and wrap them in insulation. You can also help warm them by getting into a sleeping bag with them.
Offer sugary beverages and simple sugars (like juice or candy) to help replace lost calories quickly. Warm, sugary drinks are the best option. However, it’s more important that the drink or food is sugary than warm. Once the patient’s calories have been restored and they are alert, you can encourage them to exercise.
If you are able to do this quickly, the patient will usually be re-warmed and won’t have to be evacuated. However, you should still consider your exit plan and call for help if you have any doubt.
Don’t:
- Offer caffeine or alcohol
- Try to rapidly re-warm the patient, such as by putting them in hot water
- Make the patient sit up
- Let the patient fall asleep
- Force the patient to exercise/move around before their calories have been restored
Moderate Hypothermia
Symptoms:
- Core body temperature 82-90°F
- Less shivering
- Slowed heartbeat and breathing
- May pee themselves
- May hallucinate
Treatment:
As with mild hypothermia, your first steps are to remove wet clothing. If possible, apply heat packs to major artery areas. The heat packs should be wrapped in something so they don’t burn the patient’s skin. Afterwards, you’ll need to insulate the patient by putting them in a hypothermia wrap.
It’s important that you handle the patient gently. At this stage of hypothermia, the patient’s heart has slowed down. Rough handling can cause the cardiac arrest. While it is possible to rewarm the patient, you should still plan your evacuation.
Don’t:
- Delay evacuation
- Force the patient to eat or drink
- Try to rapidly re-warm the patient
- Handle the patient roughly
Severe Hypothermia
Symptoms:
- Core body temperature less than 82°F
- Shivering stops
- Unconscious and no longer responsive
- Heartbeat is slow, faint, and may be irregular
- Slow breathing
- Stiff muscles
Treatment:
Severe hypothermia is life-threatening. There’s almost no chance that the person will be re-warmed in the field, so you will need to evacuate. To prepare the patient for evacuation, you need to get them in a hypothermia wrap. If the person’s heart stops, be prepared to perform CPR.
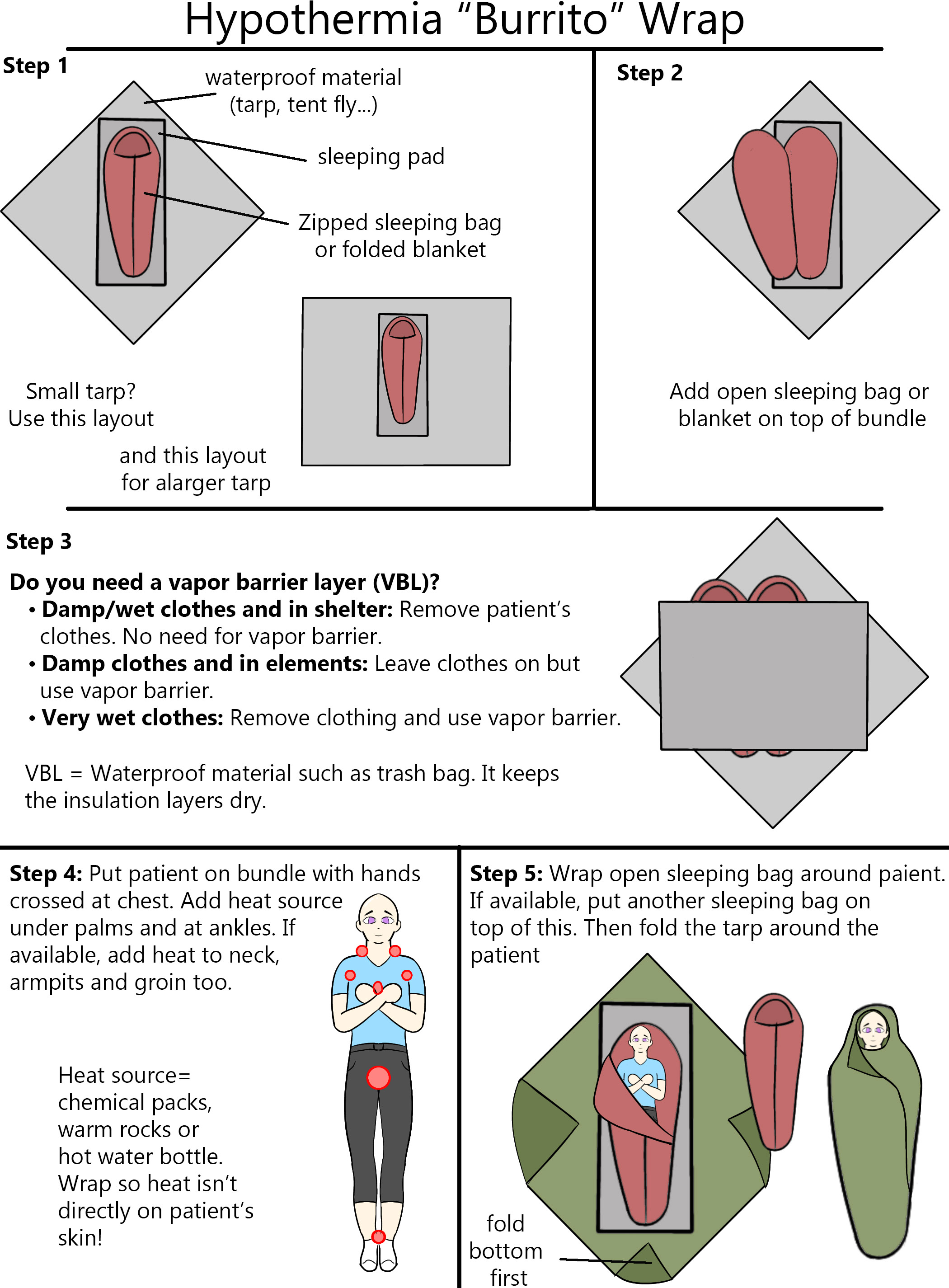
How to Do a Hypothermia “Burrito” Wrap
Notes:
- These instructions require you to have three sleeping bags or blankets. If you only have one sleeping bag or blanket, then skip steps #3 and #9. You can also use other items for insulation, such as dry spare clothing.
- The bundle should NOT be pretty. It will be huge and bulky. The more insulation, the better.
Instructions
- Lay a tarp on the ground. You can also use another waterproof material, such as a tent fly.
- Put a sleeping pad in the middle of the tarp.
- If the tarp is small, lay the pad on the diagonal.
- If the tarp is very large, lay the pad out horizontally.
- Put a zipped-up sleeping bag or blanket on the sleeping pad.
- Put an open sleeping bag or blanket on top of this.
- Add a vapor barrier liner (VBL), such as a space blanket, on top of the open sleeping bag.
- If no full-size VBL is available, consider making a “diaper” for the patient out of a trash bag.
- Lay the patient on the VBL.
- Make sure their hands are crossed at their chest
- Add a heat source to the patient’s major arteries
- Wrap the open sleeping bag + VBL around the patient.
- Put another zipped-up sleeping bag over the wrapped patient.
- Wrap the tarp around the entire bundle. Do the legs first then the sides.
- Tie up the bundle.
Applying Heat Sources
If possible, apply heat sources to the hypothermic patient. This can be a bottle of hot water, heated rocks, or chemical heat packs. The heat source should be wrapped in something so it isn’t in direct contact with the patient’s skin.
Lay the heat sources on the patient’s main arteries. The best places are:
- Under palms
- At ankles
- Behind or at sides of neck
- Armpits
- Groin
Should Someone Else Be in the Hypothermia Wrap?
It generally isn’t advised to have someone else crawl into the hypothermia wrap with the patient. While the other person’s body heat might help warm up the hypothermic patient, body-to-body warming generally isn’t very effective.
It’s harder to evacuate a two-person hypothermia wrap. You’d need to have a much larger tarp and more insulation materials to wrap two people. Even if you have all of these materials, you probably won’t be able to properly close the bundle, so heat will escape.
Further, if someone enters the bundle, that person won’t be able to help with other tasks. They’d be better off doing something like creating a fire (here’s how to do it in the rain) to boil water for heat packs (here’s how to boil snow effectively)
Do You Remove Wet Clothing from a Hypothermic Patient?
Wet clothes make hypothermia worse because evaporation will cause the patient to lose even more body heat. Because of this, it’s generally recommended to remove the patient’s wet clothing. If it’s not realistic to get them into dry clothes, you wrap the patient up naked.
However, in cold and windy environments, removing the patient’s clothing could make the heat loss worse.
Instead of removing clothing, you can wrap the patient in a vapor barrier liner (VBL), which is just a fancy way to call any waterproof material. The VBL prevents water from evaporating off of the patient’s skin, so they don’t lose more heat despite being wet. Trash bags, plastic sheeting and Mylar blankets are all examples of VBLs.
Not sure when to remove clothes or when to keep them on? Use these guidelines:
- Damp or wet clothes and the patient can get to a warm shelter quickly: Remove clothes
- Damp clothes and no shelter available: Leave clothes on and wrap patient in a VBL
- Very wet clothes: Remove clothing and use vapor barrier
Hypothermia, Urination and “Diapers”
Another benefit of using a VBL is that hypothermic patients often pee themselves, causing their insulation layers to get wet. The VBL will help keep the insulation layers dry even if this happens.
If you don’t have a large waterproof material to wrap the patient in, consider making a “diaper” for the patient out of a trash bag.
Sources:
https://pubmed.ncbi.nlm.nih.gov/25712295/
https://pubmed.ncbi.nlm.nih.gov/22445055/
https://www.ncbi.nlm.nih.gov/books/NBK545239/
https://www.realfirstaid.co.uk/hypothermia
https://blog.nols.edu/2020/2/27/treating-hypothermia-appalachian-trail
Image credit: “wrapped…” (CC BY-NC-ND 2.0) by Red Cross of Southern Missouri













Post your comments